SwiftEye Medical:
AI COVID-19 Detection
🔹 Outcome: Built a YOLOv5 model to detect COVID-19 and pneumonia from X-rays, achieving best-in-class classification accuracy.
🔹 Role & Skills: Conducted research, supported data pipeline design and ML model training, built prototype dashboard, mobile UX, and pitch deck.
🔹 Key Strengths Shown: ML prototyping, healthcare UX design, applied computer vision, impact storytelling.
Lessons Learned
Technical vs. Clinical Standards Gap: 57.76% precision excited us until radiologists said clinical deployment needs 90%+ accuracy. Technical feasibility ≠ product viability.
Dataset Limited Scope: Started wanting multi-condition detection but dataset only supported COVID classification. Learned to align technical scope with available resources upfront.
Regulatory Blindspot: Ignored FDA/HIPAA requirements in roadmap. 6-month timeline became 18+ months. Front-load compliance research in healthcare products.
1. Identifying the Problem: Slow & Inconsistent Diagnosis
Approach
To validate feasibility and user needs, we conducted data analysis, ML prototyping, and UX research to design an effective AI-driven solution.
Problem Overview
COVID-19 spreads rapidly and can cause severe respiratory complications. The current gold standard for diagnosis, RT-PCR testing, has major limitations:
Slow results: Takes 24+ hours to return findings.
Inaccuracy: 30-70% sensitivity, leading to false negatives and delayed treatment.
Limited access: Requires laboratories and trained personnel, making it difficult to scale testing in overwhelmed healthcare systems.
User Pain Points
Delays in treatment & isolation
False negatives increase spread
Limited access to rapid testing
Competitive Gaps
RT-PCR is slow and resource-heavy.
Existing imaging tools lack AI automation for detection.
Opportunity
AI-powered imaging can provide faster, scalable, and automated COVID-19 detection, improving accuracy and accessibility.
2. Developing the AI Model: Feasibility & Implementation
Technology Feasibility
AI in medical imaging: Research shows machine learning can analyze chest X-rays & CT scans for COVID-19 detection.
Comparable performance: CT scans have 98% sensitivity, X-rays 69%, making them viable diagnostic tools.
Existing gaps: Current systems lack automated classification & severity tracking.
Market Demand
COVID-19 diagnostics remains a priority: Rapid, accurate detection is essential for outbreak management.
AI adoption in healthcare is growing: Increasing investment in automation for diagnostics & triage.
Clinician need for AI support: Faster imaging-based tools can assist with triage while waiting for RT-PCR results.
Strategic Fit
Bridges a diagnostic gap: Faster and more accessible alternative to slow lab-based testing.
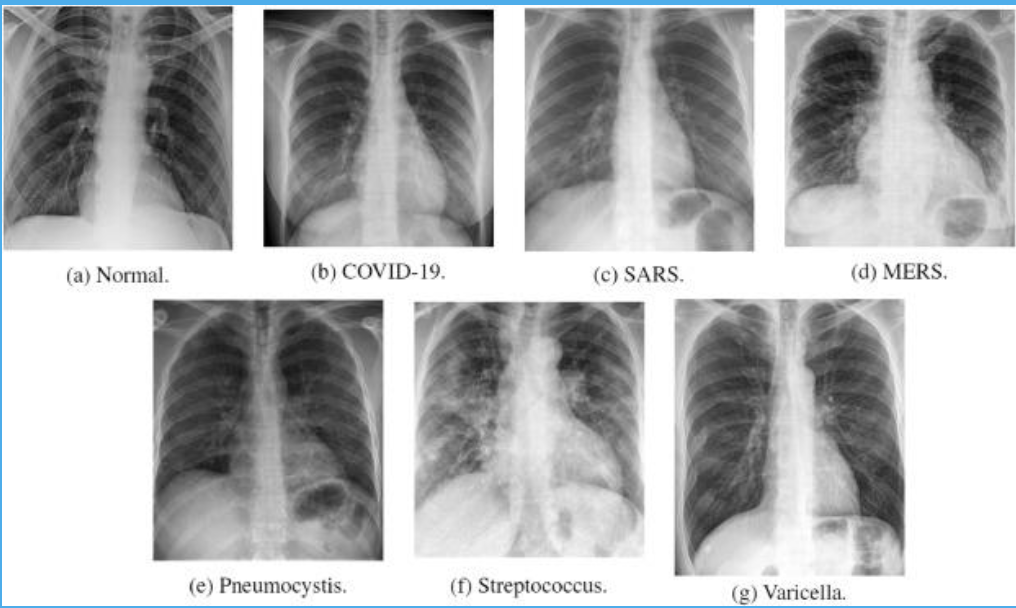
Scalable beyond COVID-19: Potential for pneumonia detection & broader AI-driven radiology applications.
Opportunity
An AI-powered COVID-19 diagnostic tool can enhance screening speed, reduce reliance on RT-PCR, and improve decision-making for healthcare professionals.
3. Prototyping the AI-Powered COVID-19 Detection System
Building & Evaluating Machine Learning Models
To develop an AI-powered COVID-19 detection system, we focused on:
Preprocessing chest X-ray datasets for training deep learning models.
Prototyping & optimizing object detection models (YOLO v5, Faster R-CNN).
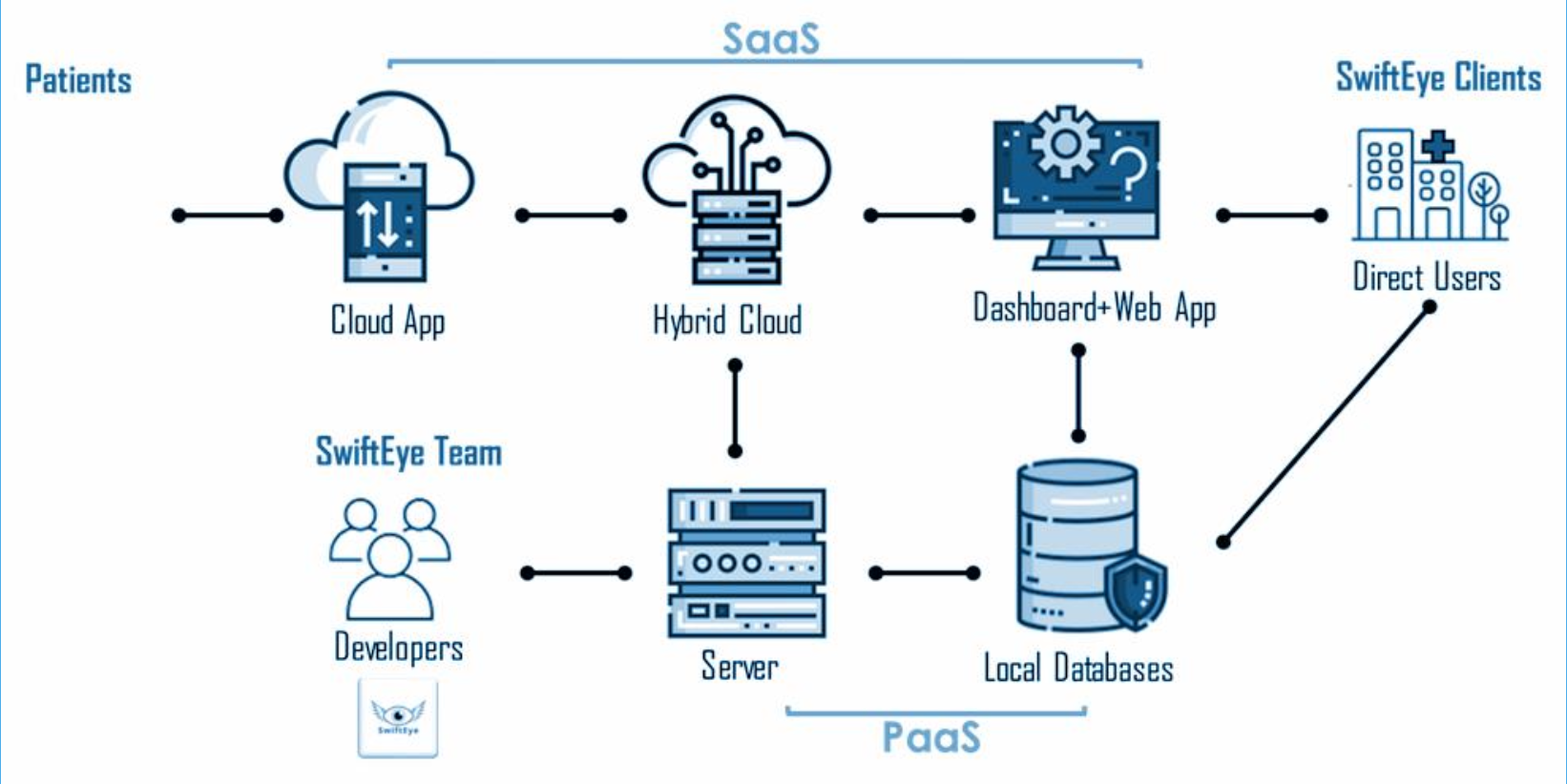
Designing an analytics dashboard & mobile app prototype for usability testing.
Machine Learning Development & Model Performance
Data Collection & Preprocessing
Sourced chest X-ray datasets from medical repositories.
Resized images (512x512, 256x256 pixels) to optimize training.
Applied data augmentation to improve generalization.
Model Training & Evaluation
Two deep learning architectures were tested:
YOLO v5: Optimized for real-time detection.
Faster R-CNN: Enhanced lesion segmentation.
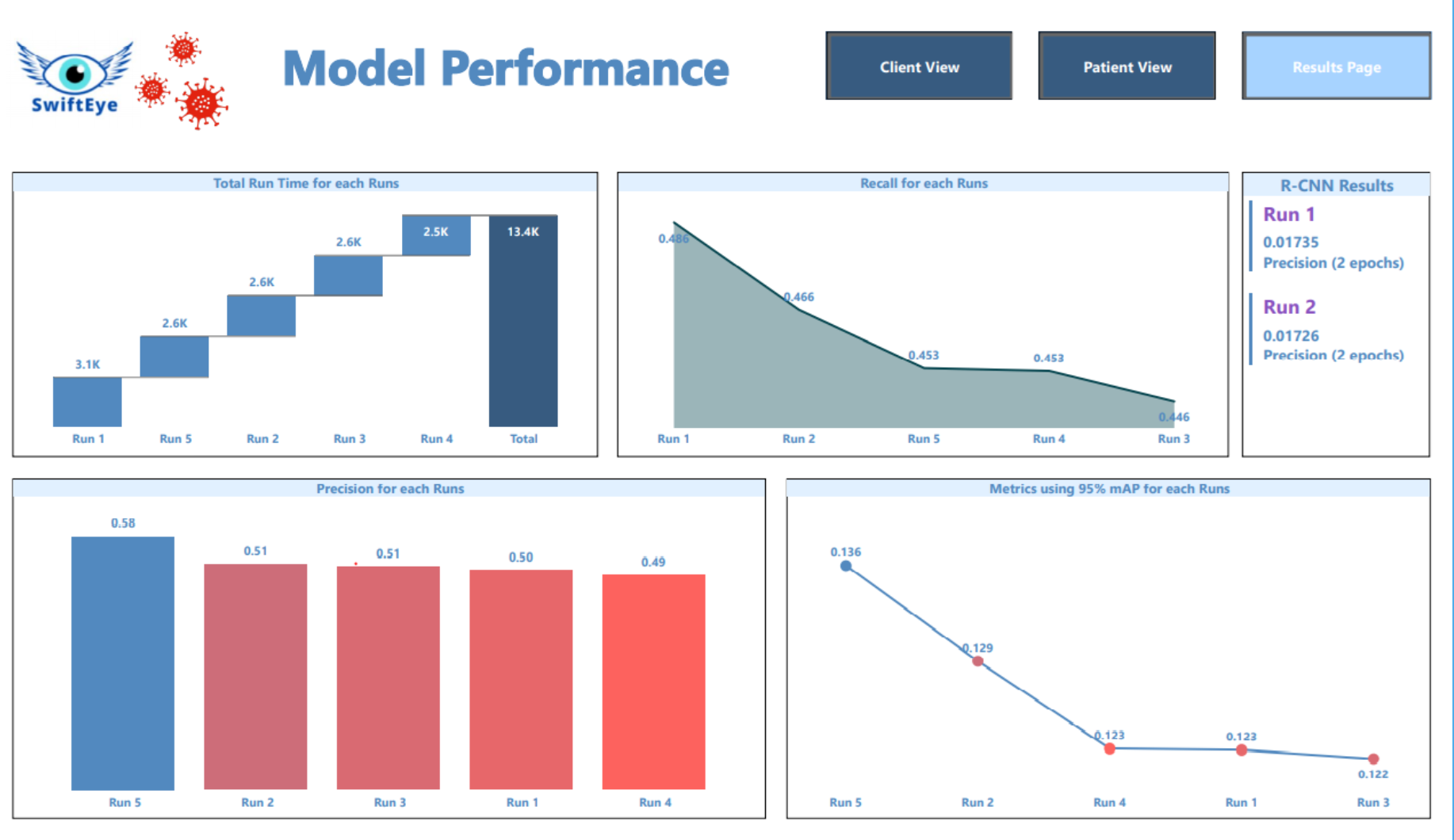
Model Performance & Insights
YOLO v5 Model 5 (512x512 resolution) was the optimal model, achieving:
Precision: 0.5776 (strong performance in identifying COVID-19 positive cases).
Mean Average Precision (mAP@0.5): 0.4543, indicating the model successfully identified affected lung regions in over half of the images.
Hyperparameter Optimization:
Trained models for 50 epochs (Run 6 extended to 75 epochs for minimizing underfitting).
Adjusted learning rate, momentum, and weight decay to improve convergence & reduce overfitting.
Key Takeaway:
The optimal YOLO v5 model can assist radiologists as a decision-support tool, identifying lung abnormalities efficiently within a human-in-the-loop workflow.
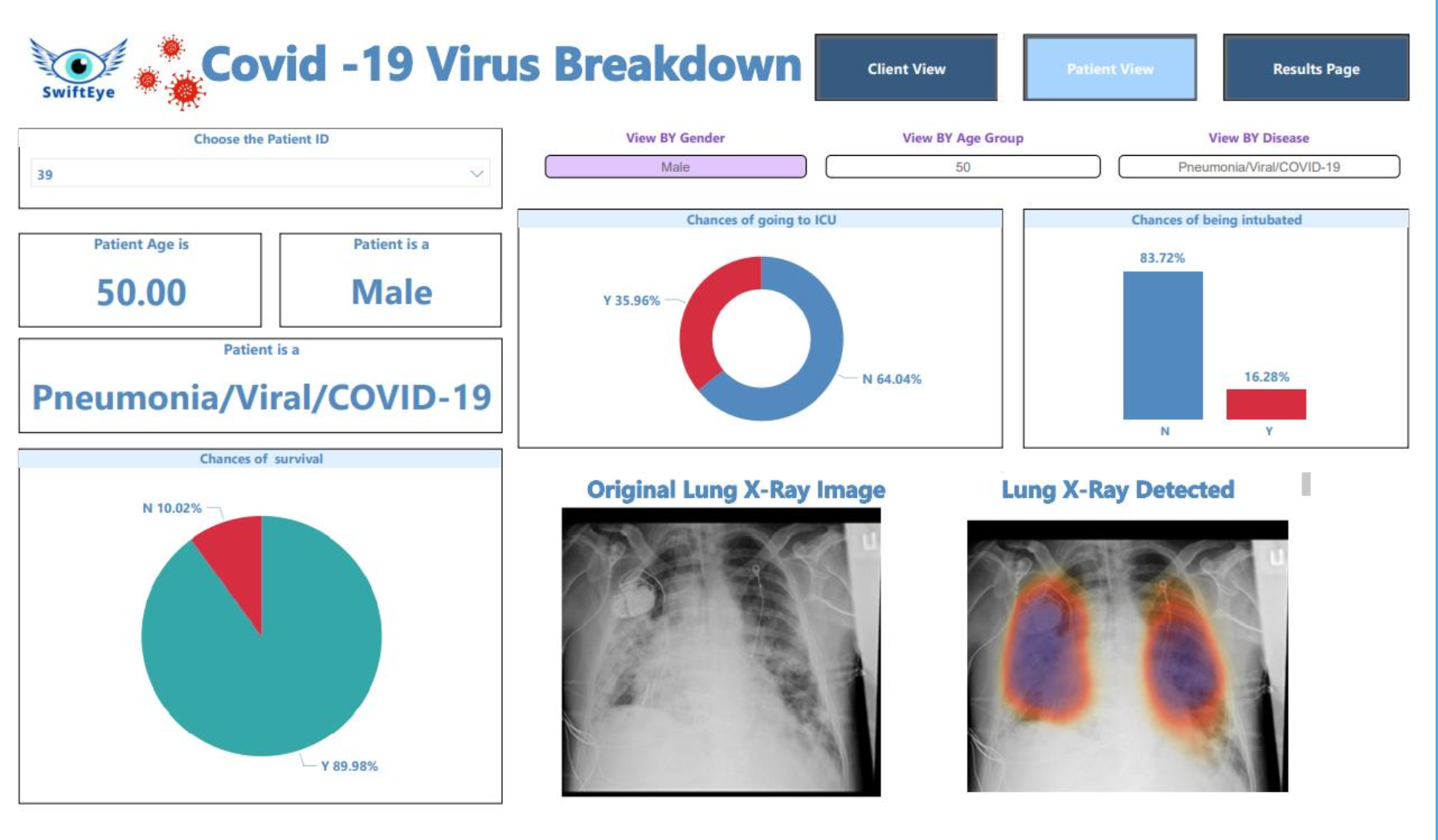
Application: Conceptualizing a Doctor-Facing Analytics Tool
Beyond model development, we explored how AI could be integrated into clinical workflows through an interactive dashboard & mobile app prototype:
Real-time X-ray analysis & severity scoring to assist radiologists.
Trend visualization & predictive insights for patient monitoring.
User-friendly mobile interface for rapid screening in remote/hospital settings.
This phase validated AI’s feasibility for COVID-19 detection, laying the groundwork for further development, regulatory approval, and clinical integration.
4. Roadmap & Implementation Strategy
To structure development and deployment, I aligned the roadmap with a phased approach, prioritizing technical feasibility, clinical validation, and adoption.
Phase 1: Data Collection & Model Prototyping (Completed)
Objective: Establish technical feasibility through dataset preparation and AI model development.
Collected & Preprocessed X-ray Data: Standardized imaging formats for training.
Trained YOLO v5 & Faster R-CNN Models: Iterated on hyperparameters for optimal COVID-19 detection.
Validated Model Performance: Identified YOLO v5 Run 5 as the best-performing model for clinical applications.
Phase 2: Model Testing & UX Design (Completed)
Objective: Validate model accuracy and conceptualize user-facing solutions.
Tested Models on Various Resolutions: Assessed trade-offs in accuracy & processing speed.
Developed Model Interpretability Tools: Enabled transparency in AI-driven decisions.
Designed AI-Powered Dashboard & Mobile Prototype: Conceptualized doctor-facing UI for real-time analysis.
Phase 3: Clinical Validation & Feedback Iteration (Future Work)
Objective: Ensure real-world clinical adoption through testing and compliance.
Pilot Testing with Radiologists: Evaluate AI-assisted workflows in hospitals.
Refine Model with Clinician Feedback: Improve accuracy & usability based on real-world testing.
Address Regulatory & Compliance Needs: Align with FDA & HIPAA standards for AI-driven diagnostics.
Phase 4: Deployment & Scalability (Future Work)
Objective: Expand adoption and integrate AI into broader radiology applications.
Expand to Additional Imaging Modalities: Adapt AI for CT scans & lung ultrasounds.
Develop Full-Scale SaaS Platform: Integrate AI-powered diagnostics into hospital IT systems.
Enable Continuous Model Learning: Implement real-world data feedback loops for continuous improvement.
Key Takeaways: How This Showcases My Product Thinking
AI-Driven Feasibility Testing
Validated model performance across multiple architectures & hyperparameters.
Human-Centered Design
Designed UX prototypes tailored for radiologists & frontline healthcare workers.
Scalable Roadmap
Defined phased implementation strategy for AI integration in real-world clinical settings.